Types Of Toenail Fungus Uncovered: Causes, Symptoms, and Treatment Tips
Table of Contents
Toggle
Toenail fungus, also known as onychomycosis or tinea unguium, is a common yet often underestimated problem that affects millions worldwide. It often starts as a yellowish or white superficial spot under the nail and can progress into a severe fungal nail infection if untreated. The fungus thrives in damp and dark environments, such as sweaty shoes or public spaces like a nail salon. Over time, this condition can lead to thick, brittle nails with yellowish-brown discoloration, streaks, or even complete loss of the nail. In some cases, it may affect the tissue underneath, causing pain, nail deformity, and additional symptoms.
Based on my experience working with podiatrists and clients across Miami, Pembroke Pines, and Broward County, I’ve seen how essential early treatment is. Experts often recommend oral anti-fungal medication or advanced therapies like laser treatment for subungual infections or candida. While the toenails are most frequently targeted, fingernails are also at risk, particularly in regions like South Florida, where the warm, humid climate creates the perfect environment for the growth of microorganisms like mold. Clinics in areas like Miami Beach, Hollywood, Coral Gables, Kendall, and Boca Raton offer specialized care to address this condition, ensuring the infection doesn’t escalate into something more noticeable or difficult to manage.
Types Of Toenail Fungus
Toenail fungus can take many forms, but the most common types arise from fungal infections that impact the nails and the surrounding skin.
- One such infection, subungual onychomycosis, is often caused by dermatophytes, a class of fungi that also triggers Athlete’s Foot.
- These infections can develop underneath the nail, either near its base (referred to as proximal subungual onychomycosis) or toward the distal edge (distal subungual onychomycosis).
- Another form, white superficial onychomycosis, primarily affects the outer layer of the nail and appears superficial.
- In some cases, candida onychomycosis, which is linked to the overgrowth of candida yeast, can lead to visible changes in the appearance of the nail.
These infections are influenced by the surrounding environment, entering through cracks in the nail or skin. With over 40 species of fungi, grouped into genera like microsporum, epidermophyton, and trichophyton, these infections vary in their symptoms, causes, and impact on individuals.
1.Subungual Onychomycosis: Common and Rare Forms
Subungual Onychomycosis:
Subungual onychomycosis, a fungal infection targeting the nail bed and nail plate, is one of the most prevalent types of toenail fungus. It often begins as a yellowish spot near the edges or the nail tip, gradually spreading toward the center and affecting the keratin-producing structures of the nail matrix. This condition is frequently caused by Trichophyton rubrum, a type of fungus within the dermatophyte class. In some cases, other fungal species, like Fusarium and Acremonium, can also cause infection. For those with a compromised immune system, such as individuals with HIV or human immunodeficiency virus, the infection may start at the base of the nail, resulting in proximal subungual onychomycosis.
Distal Lateral Subungual Onychomycosis (DSLO):
Less commonly, forms like distal lateral subungual onychomycosis (DSLO) impact the sides or tips of the nails, often causing symptoms such as crumbling, discoloration, or even lifting of the nail. Dermatophytes, such as epidermophyton and microsporum, are among the 40 genera of fungi known to infect these areas. These infections can cause the nail to thicken and appear discolored, especially if left untreated. Although the condition is commonly associated with an athlete’s foot, the infection is less likely to begin on healthy skin or hair follicles.
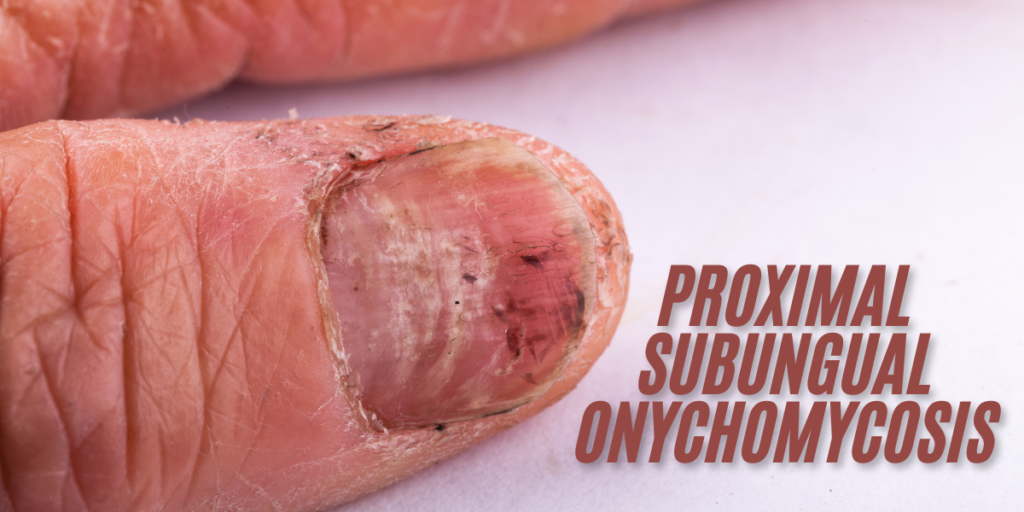
2.Proximal Subungual Onychomycosis: A Rare and Challenging Condition
Proximal subungual onychomycosis, often abbreviated as PSO, is a rare type of toenail fungus that begins at the base of the nail, near the lunula, a half-moon-shaped structure. This condition is caused by the organism Trichophyton rubrum and typically affects individuals with weakened immune systems, such as those living with HIV or HIV/AIDS. Unlike more common infections, PSO is often reported in cases where individuals are undergoing treatment with TNF-α inhibitors or methotrexate. Studies by Andersen PL, Henning MAS, and Jemec GBE in 2018, published in Acta Dermatovenerol Croat, have documented its impact and challenges in treatment.
Progression and Symptoms:
The infection usually starts as white spots on the nail bed or cuticle and spreads outward as the toenail or fingernail grows, often involving the proximal nail fold. In severe cases, it can affect the top of the foot. Though rare, with only about 20 out of every 100 reported cases, PSO has significant implications. Dermatophytes are commonly linked to infections in nails, including toenails, fingernails, and nail beds, accounting for over 70% of fungal infections. Early identification and effective treatment are essential to address these issues in the affected area.
3.White Superficial Onychomycosis (WSO)
White superficial onychomycosis (WSO) is an uncommon type of toenail infection that affects only the top layer of the nail. This condition is caused by fungi such as Trichophyton mentagrophytes and other species like Fusarium and Aspergillus. WSO accounts for about 10% of all reported cases of onychomycosis. It starts as white spots on the nail’s surface, which later become soft, powdery, and prone to crumbling, leaving the nail with a rough, flaky texture.
Symptoms and Treatment:
The infection is relatively easy to treat because it remains confined to the top layer of the nail, unlike other fungal infections that penetrate deeper. Symptoms include pitting, well-defined patches, and eventually a crumbly surface. Studies by experts such as Leung, Lam, and Leong in 2020 have emphasized the importance of early detection. If untreated, the infection can spread across the entire nail, making treatment more difficult. With over 1,000 species of Fusarium and 100 species of Acremonium, WSO stems from a variety of causes, but early intervention ensures effective
4.Candidal Nail Infections
Candidal onychomycosis, caused by Candida albicans, is a less common but distinct type of fungal infection that affects the toenails or fingernails. This condition is often triggered by factors such as diabetes, an impaired immune system, or HIV infection.
Symptoms:
Symptoms include inflamed, reddish areas around the nail, and in severe cases, the entire nail may detach due to the breakdown of the nail surface, leaving behind rough or pitted nails.
Causes and Progression:
Common causes include exposure to wet feet, detergents, or harsh chemicals like soaps, especially among individuals working in such environments. In some cases, the infection is linked to chronic mucocutaneous candidiasis and may progress rapidly, affecting soft tissues and penetrating deeper structures like the GI tract or mucus membranes. This condition is marked by swelling, opalescent discoloration, and circulation problems, making it harder to manage, particularly in individuals using immunosuppressant medications. Visual examples by photographers such as Luliia Petrovskaia (found on platforms like Getty Images) highlight severe cases where nails become edematous, brittle, and significantly damaged following an injury or prolonged neglect.
Toenail Fungus: Symptoms and Progression
Initial Symptoms:
Toenail fungus often begins with white or yellow spots appearing on the surface of the nail. These spots may spread, leading to discoloration that ranges from green to black. Over time, the nail may thicken, become brittle, or start to crumble under pressure. In some cases, the nail might loosen or even separate entirely from the nail bed. Other common signs include a bad smell, a build-up of debris, or dark spots beneath the nail.
Advanced Symptoms and Complications:
As the infection worsens, the nail may become misshapen, making it hard to trim or manage. You might experience pain or pressure, especially when walking, and notice curling or further crumbling of the affected nails. Symptoms can include browning or yellowing patches, as well as subungual changes, such as debris collecting under the nail. Whether caused by yeast, mold, or another fungal agent, recognizing these signs early is critical to preventing long-term damage.
Impact on Daily Life:
The severity of symptoms often varies, but if left untreated, toenail fungus can become a major inconvenience. What starts as a mild issue can escalate into difficulty performing daily activities due to discomfort and changes in the nail’s appearance. Monitoring for unusually shaped nails and seeking treatment promptly is essential to controlling the infection.
Causes and Risk Factors of Toenail Fungus
Fungal Growth and Entry:
Toenails are particularly vulnerable to fungus due to their exposure to moist, hot, and sweaty places, such as gym showers, pools, and swimming areas. Fungi like Trichophyton rubrum, Microsporum, and Scopulariopsis thrive in these environments and easily enter through cracks in the skin or nails, especially in adults with brittle or damaged toenails.
Contributing Medical Conditions:
Infections may worsen when combined with medical conditions like psoriasis, Darier disease, or reduced blood circulation. Males and individuals who wear gloves or keep their hands wet for extended periods are at greater risk. Some fungal types, including Paecilomyces, Neoscytalidium, and tropicalis, are resistant to standard treatments such as antifungal creams or laser therapy.
Complications and Prevention:
Secondary infections, including bacterial infections like chloronychia or green-nail syndrome, can cause additional discoloration or wart-like symptoms. Preventive measures, such as maintaining proper hygiene and avoiding contaminated places, can reduce the risk of infections caused by fungi like Alternaria, Soudanense, and Onchocola. Left untreated, these infections can lead to severe complications requiring surgery or advanced remedies.
Medical and Genetic Factors:
Toenail fungus is more likely to occur in individuals with a family history of nail infections or a history of athlete’s foot. Those with a weak immune system, whether due to HIV, cancer, or the use of immunosuppressants like chemotherapy, are particularly vulnerable. Conditions such as diabetes, psoriasis, or poor circulation caused by peripheral vascular disease increase the risk, often due to reduced blood supply, slow-growing nails, and a diminished ability to fight infections.
Lifestyle and Environmental Factors:
Lifestyle choices and environmental exposure also play a significant role. Spending time in damp areas like indoor swimming pools, excessive sweating, smoking, or wearing poor-fitting shoes can increase the chances of infection. Physical trauma, such as injuries or surgeries, can create openings for fungal infections to develop. People with skin conditions, including those with silvery scales, itchy patches, or red patches, are at a higher risk. Once the infection sets in, trapped dirt and debris around the nails can worsen the problem, leading to further complications.
Diagnosing and Treating Toenail Fungus
Importance of Early Diagnosis:
When addressing fungal infections of the toenail, early diagnosis is essential for effective treatment. A podiatrist, experienced in nail and foot care, will carefully examine the nail to evaluate visible symptoms and determine the exact type of fungus. In some cases, the infection may mimic other conditions, such as psoriasis, or involve bacterial or yeast elements, making precise testing crucial.
Diagnostic Process:
The diagnosis typically involves scraping or clipping a small sample of the affected nail. This sample is analyzed under a microscope to confirm the presence of a fungal infection. If the initial results are negative, a culture test may be performed to observe if the fungus grows under controlled conditions. Based on the findings, the podiatrist will create a personalized treatment plan, which may include prescription medications.
Guidance and Resources:
Following the advice of a trusted podiatrist and adhering to their recommendations can significantly improve treatment outcomes.
Treating Toenail Fungus
Prescription Medications:
Prescription medications are often the foundation of treating toenail fungus. Among oral options, terbinafine (Lamisil) and itraconazole (Sporanox) are commonly prescribed for stubborn nail infections. These medications work deep within the nail to eliminate the fungus, but they may require months of treatment. Regular blood samples are taken to monitor potential side effects, such as liver abnormalities or nausea. For individuals unable to tolerate oral medications, topical antifungals like efinaconazole, ciclopirox, and tavaborole are available. These treatments are applied directly to the nail and surrounding skin and are more effective for mild or superficial cases.
Combination Treatments and Advanced Options:
For severe or resistant infections, healthcare providers may combine oral and topical medications to enhance effectiveness. Studies, including F1000Research and research like Rev-968, highlight evolving strategies in managing fungal infections. Common challenges include side effects such as itching, redness, and burning. In extreme cases of nail deformation or malformed nails, a minor procedure under local anesthesia may involve removing the affected nail to aid healing. Experts, like Gupta, emphasize the importance of a proper diagnosis in a certified laboratory to ensure the best treatment plan and prevent complications.
Managing Toenail Fungus with Home Remedies
General Hygiene and Maintenance:
Dealing with toenail fungus can be challenging, especially when symptoms are mild yet persistent. While medical treatments are often recommended, home remedies can support the treatment process.
- Start by keeping your toenails clean and dry, as moisture encourages fungal growth.
- Regular cleaning, disinfecting socks, and shoes are simple yet effective habits.
- Using a nail-softening cream can make filing affected areas easier, helping anti-fungal topical treatments penetrate deeper into the nail.
- Over-the-counter (OTC) ointments are another popular option for addressing infections.
Natural Remedies and Additional Care:
Some home remedies involve natural ingredients. Baking soda can absorb moisture, while vinegar and hydrogen peroxide may create an environment that inhibits fungal growth. Others turn to mentholated ointments, containing menthol, eucalyptus oil, or camphor, to soothe affected areas and support treatment. While the effectiveness of these remedies remains uncertain, being diligent in your care routine may help reduce the spread of the fungus and improve overall nail health.
Treating Severe or Subungual Infections
Managing the Infection:
Severe or subungual infections require a more persistent and targeted approach. Regular trimming and filing of the nail can help make the infection more accessible to anti-fungal creams. However, larger or slow-growing toenails may take months, sometimes up to 12 months, for the affected parts to grow out completely.
Combining Treatments for Better Results:
Incorporating home remedies alongside professional guidance from a doctor can help reduce the infection’s spread and promote healing. In some cases, creating a dry and inhospitable environment might be sufficient to eliminate the fungus, though this is not always guaranteed.
Preventing Toenail Fungus and Maintaining Healthy Nails
Hygiene and Nail Care:
To keep your toenails healthy and free from infection, prioritize proper hygiene. Always keep your nails trimmed, clean, and avoid excess moisture. Ensure that you clean and disinfect your trimmer after every use, and skip using nail polish if your nails are damaged. When visiting salons, confirm that they have a valid license, sterilize their tools, or bring your own file to reduce risks.
Protective Measures and Daily Habits:
In communal spaces like public showers, pools, or locker rooms, wear flip-flops or thongs to shield your nails and skin from fungi. For individuals managing diabetes or other health conditions, apply antifungal sprays or powders as a preventive measure. Choose breathable shoes and socks to keep your feet and toes dry, and avoid loose footwear that can cause trauma or breaks.
Nighttime and Long-Term Care:
Before bed, apply nourishing oils or therapy creams to encourage healthy nail growth, and let your feet rest without occlusive footwear. If dealing with an ongoing issue, focus on cleaning, soaking your feet in warm water, and following the advice of healthcare providers. Adopting these simple daily habits can target the factors contributing to nail problems, helping you maintain strong and healthy nails.
Understanding the Risks of Toenail Fungus
Potential Complications:
Toenail fungus, often dismissed as merely unsightly or harmless, can lead to serious complications if untreated. Fungal infections can cause nails to become discolored, misshapen, and even painful. For individuals with underlying health conditions like diabetes, the risks are heightened. Diseases such as peripheral and vascular conditions can reduce blood flow to the extremities, impairing the body’s ability to fight infections. This slowed healing process allows the fungus to spread further, potentially requiring prolonged therapy. Left unaddressed, the infection may cause nails to look permanently damaged or take over a year to fully recover, even with proper treatment.
Causes and Professional Care:
Physical trauma to the nail creates openings for dirt and debris to accumulate, increasing the likelihood of fungal growth. A healthcare provider, such as a podiatrist, is crucial in managing these complications. They can develop targeted treatment plans to address the infection and prevent recurrence or systemic concerns. Trusted resources like MedlinePlus emphasize the importance of early intervention, as prolonged infections may require intensive care. Addressing these issues promptly helps reduce the severity of cases, allowing the body time to recover and regain its healing capacity.
When to See a Doctor for Toenail Fungus?
Toenail fungus is a persistent problem that starts when microorganisms enter through small injuries or damage to your toenails. The infection often spreads, leading to noticeable changes in the nail, such as discoloration and thickening. If left untreated, the fungi can worsen and cause discomfort. While it may seem impossible to manage this condition at home, consulting a healthcare provider can offer effective treatment options.
To reduce risk and prevent future infections, it’s essential to stay aware of contributing factors like maintaining clean and well-protected feet. Regularly keeping your toes dry and ensuring proper hygiene can go a long way in treating and avoiding reinfections.